In the realm of aesthetic medicine, the quest for beauty and self-improvement is often intertwined with complex ethical dilemmas. As practitioners, we are tasked with navigating these challenges while ensuring the safety and well-being of our patients. This becomes particularly crucial when dealing with vulnerable groups such as adolescents, the elderly, those with psychological vulnerabilities, and individuals from culturally diverse backgrounds. How can we balance respect for autonomy with the imperative to protect these individuals? Let’s embark on a journey through the ethical labyrinth to find the answers.
The Adolescent Conundrum
Adolescence is a period marked by rapid physical and psychological changes, making it a particularly sensitive time for aesthetic interventions. The ethical challenge lies in distinguishing between genuine medical needs and the pressures of societal beauty standards.
Consider the case of a 16-year-old seeking rhinoplasty. Is this a decision driven by personal desire, or is it influenced by peer pressure and media portrayals of beauty? The ethical practitioner must delve deeper, engaging in thorough consultations to understand the motivations behind the request.
A robust ethical framework for adolescents includes:
- Informed Consent: Ensuring that the adolescent fully understands the procedure, its risks, and its long-term implications. This often involves involving parents or guardians in the decision-making process to provide additional support and oversight.

- Psychological Assessment: Conducting a comprehensive psychological evaluation to assess the adolescent’s readiness for the procedure and to identify any underlying issues that may be driving the request.
-
Long-Term Impact: Considering the potential long-term effects on the adolescent’s physical and psychological development. Procedures that may seem beneficial in the short term could have unforeseen consequences as the individual matures.
By implementing these measures, practitioners can better navigate the ethical complexities of adolescent aesthetic medicine, ensuring that decisions are made in the best interest of the patient.
The Elderly: Balancing Enhancement and Health
As individuals age, the desire to maintain a youthful appearance can lead them to seek aesthetic interventions. However, the ethical considerations for the elderly are multifaceted, requiring a delicate balance between enhancing appearance and safeguarding health.
Imagine an 80-year-old patient requesting a facelift. On one hand, such a procedure could significantly improve their quality of life by boosting self-esteem and social engagement. On the other hand, the risks associated with surgery are heightened due to age-related health issues.
Ethical considerations for the elderly include:
- Health Assessment: Conducting a thorough medical evaluation to assess the patient’s overall health and their ability to withstand the stresses of surgery. This may involve consultations with other healthcare professionals to ensure a comprehensive understanding of the patient’s health status.

- Realistic Expectations: Setting clear, realistic expectations about the outcomes of the procedure. It is crucial to manage the patient’s expectations and ensure they understand that aesthetic interventions can enhance but not reverse the aging process.
-
Alternative Options: Exploring non-invasive or less risky alternatives that could achieve similar results. For example, dermal fillers or laser treatments might offer a safer path to aesthetic enhancement.
By prioritizing the patient’s health and well-being, practitioners can ethically navigate the complexities of aesthetic medicine for the elderly, providing treatments that enhance life without compromising safety.
Psychological Vulnerabilities: The Ethical Imperative to Protect
Individuals with psychological vulnerabilities, such as those suffering from body dysmorphic disorder (BDD) or depression, present unique ethical challenges in aesthetic medicine. The practitioner’s role extends beyond mere technical expertise to encompass a deep understanding of the psychological factors at play.
Consider a patient with BDD who is fixated on perceived flaws and seeks multiple aesthetic procedures to address them. The ethical dilemma here is whether to proceed with the requested interventions or to prioritize the patient’s mental health.
Key ethical considerations for psychologically vulnerable patients include:

- Psychological Evaluation: Conducting a thorough psychological assessment to identify underlying mental health issues that may be driving the patient’s desire for aesthetic interventions. This may involve collaboration with mental health professionals to develop a comprehensive care plan.
-
Therapeutic Interventions: Prioritizing therapeutic interventions over aesthetic procedures when appropriate. For example, cognitive-behavioral therapy (CBT) may be more beneficial for a patient with BDD than repeated cosmetic surgeries.
-
Ethical Decision-Making: Engaging in a collaborative decision-making process that involves the patient, their family, and mental health professionals. This ensures that decisions are made with the patient’s best interests at heart, balancing autonomy with protection.
By adopting a holistic approach that addresses both the aesthetic and psychological needs of vulnerable patients, practitioners can navigate the ethical complexities of aesthetic medicine with sensitivity and care.
Cultural Diversity: Respecting Differences in Aesthetic Values
In an increasingly globalized world, practitioners of aesthetic medicine must be attuned to the cultural diversity of their patients. Different cultural backgrounds can significantly influence perceptions of beauty and the desire for aesthetic interventions, adding another layer of ethical complexity.
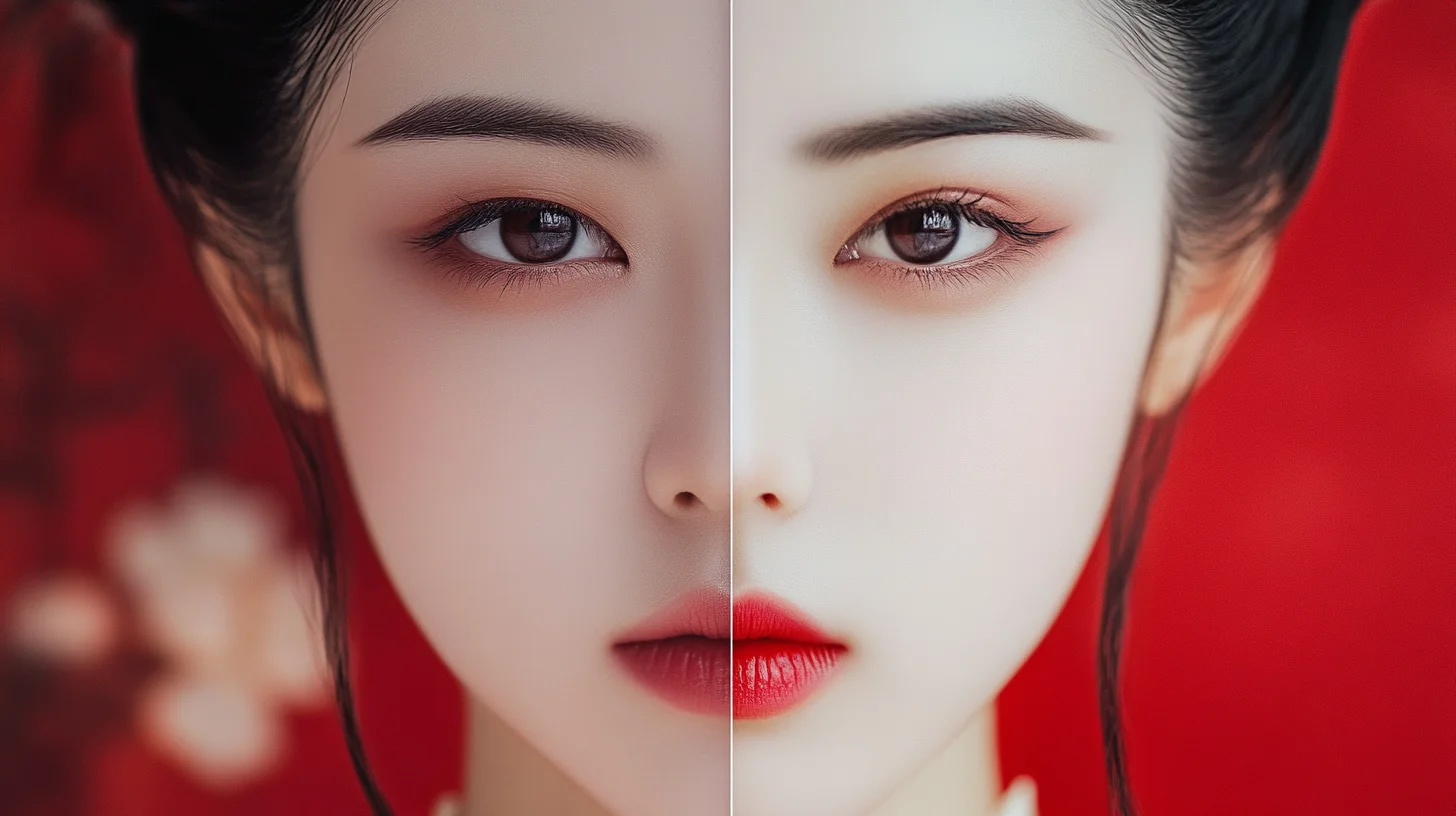
Consider a patient from a culture that values certain facial features more than others, seeking a procedure to align with these cultural ideals. The ethical challenge is to respect the patient’s cultural values while ensuring that the intervention is safe and appropriate.
Ethical considerations for culturally diverse patients include:
- Cultural Competence: Developing a deep understanding of the cultural values and beliefs that may influence a patient’s desire for aesthetic interventions. This involves ongoing education and training to enhance cultural sensitivity and awareness.
-
Respect for Autonomy: Respecting the patient’s autonomy and cultural values while ensuring that they are making informed decisions. This may involve engaging in culturally sensitive consultations to fully understand the patient’s motivations and expectations.
-
Ethical Dialogue: Fostering open and honest dialogue about the potential risks and benefits of the procedure, taking into account the patient’s cultural context. This ensures that the patient is fully aware of what the intervention entails and can make an informed decision.
By embracing cultural diversity and engaging in ethical dialogue, practitioners can navigate the complexities of aesthetic medicine with respect and sensitivity, ensuring that all patients receive the care they need and deserve.

Conclusion: The Path Forward
Navigating the ethical labyrinth of aesthetic medicine requires a deep commitment to the principles of autonomy, beneficence, and non-maleficence. By adopting a nuanced and sensitive approach to the needs of vulnerable groups—adolescents, the elderly, those with psychological vulnerabilities, and individuals from diverse cultural backgrounds—practitioners can provide ethical, compassionate care that enhances the lives of their patients.
The journey through the ethical labyrinth is not without its challenges, but it is a journey worth undertaking. By embracing these challenges and striving for ethical excellence, we can ensure that aesthetic medicine remains a field dedicated to the well-being and dignity of all individuals.